33 year old male with history of pus oozing from left upper third molar region
THIS IS AN ONLINE E LOGBOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT
CASE HISTORY:
A 33 YEAR OLD MALE AUTO DRIVER BY OCCUPATION CAME TO THE HOSPITAL WITH THE CHIEF COMPLAINTS OF PUS OOZING OUT FROM THE LEFT UPPER MOLAR REGION ON 10 OF FEB 2022
HISTORY OF PRESENT ILLNESS:
PATIENT WAS APPARENTLY ASYMPTOMATIC 60 DAYS BACK THEN HE DEVELOPED PAIN, SWELLING AND CREAM COLOURED PUS DISCHARGING FROM THE LEFT UPPER THIRD MOLAR REGION WHICH IS SUDDEN IN ONSET.THEN HE VISITED A DENTIST FOR WHICH HE PRESCRIBED MEDICATIONS AND THEN THE PAIN, SWELLING AND PUS DISCHARGE GOT RESOLVED.
AFTER 5 DAYS OF THE MEDICATIONS THE PATIENT AGAIN DEVELOPED PAIN AND SWELLING IN THE SAME REGION AND AGAIN VISITED THE DOCTOR AND CONTINUED THE MEDICATIONS . DURING THE 2 ND COURSE OF MEDICATIONS THE QUANTITY OF THE PUS IS INCREASED WITH REDUCED PAIN AND SWELLING . DURING HIS COURSE HE NOTICED THE BLOOD STAINS IN THE NOSTRILS. HE AGAIN CONSULTED THE DOCTOR AND THE DOCTOR CLEANED HIS TEETH AND THE DISCHARGE HAS BEEN REDUCED TO SOME EXTENT.DOCTOR GAVE HIM MEDICATIONS AND ORDERED OPG AND CBCT BUT PATIENT DIDN'T TAKE THE TESTS. PATIENT VISTED ANOTHER DOCTOR THIS TIME AND HE GAVE TAB.METROGYL 200MG ,CLAVAM 625MG ,VOVERAN D FOR 5 DAYS. AFTER THE TESTS DR. PRESCRIBED TAB. TAXIM O FOR 5 DAYS BUT THE PATIENT DID NOT TAKE THE TABLET THEN HE NOTICED REDDISH PUS COMING SO HE TOOK THE TABLET. LATER HE PRESENTED TO OUR HOSPITAL.
SWELLING ON THE LEFT SIDE - EFFECTED SIDE
PATIENT HAS NOT DEVELOPED THE WISDOM TEETH ON BOTH SIDES OF THE UPPER JAW.
HISTORY OF TRAUMA TO THE LEFT EYE WITH A SHARP OBJECT - KNIFE WHEN HE WAS ONE AND HALF YEARS OLD . NO SURGERY HAS BEEN DONE THEN HE LOST COMPLETE VISION OF THE LEFT EYE.
HISTORY OF TRAUMA TO THE LEFT LOWER JAW DURING A FIGHT WITH HIS COUSIN 7 YEARS BACK.
NO HISTORY OF HYPERTENSION
NO HISTORY OF DIABETES
NO HISTORY OF ASTHMA
NO HISTORY OF EPILEPSY
NO HISTORY OF TUBERCULOSIS
PERSONAL HISTORY:
APPETITE: NORMAL
DIET: MIXED
SLEEP IS ADEQUATE
NO ALLERGIES
ADDICTIONS: SMOKING , ALCOHOL AND TOBACCO OCCASIONALLY
FAMILY HISTORY: NO SIGNIFICANT FAMILY HISTORY
GENERAL EXAMINATION: PATIENT WAS CONSCIOUS , COHERENT COOPERATIVE AND WELL ORIENTED TO TIME ,PLACE AND PERSON.
WELL BUILT AND NOURISHED
BP - 110/80 mmHg, RR - 20cpm,PR- 68BPM
SYSTEMIC EXAMINATION:
- RBS - 154mg/dl, S. creatinine - 0.8, Na+ - 132, K+ - 3.8, Cl- - 98, Blood urea - 12mg/dl
- LFT : TB - 0.97, DB - 0.20, AST - 29, ALT - 159, TP - 6.8, Alb - 4.2, A/G - 1.62
- Serology -ve
- Hemogram : Hb - 15.4g/dl, TLC - 7,500 cells/cumm, PLT - 2.5 lakhs/cumm
- CUE : Alb-nil, Pus cells- 3 to 4, Epithelial cells - 2 to 4
CECT NECK
- The left maxillary sinus is narrowed by the above lesion and shows retained secretion/ mucosal thickening
- Rest of the paranasal sinus normal
- Enlarged left eyeball with a focal posterior protrusion - Staphyloma. Rest of the orbit normal
- Radiographic features can be suggestive of left maxillary sinusitis with ?osteomyelitic changes in the left floor and the medial and lateral borders of the maxillary sinus.
- D/D: Suspected aggressive lesion?
- Oro antral communication distal to #28 region
- Pulpal calcification in the teeth of the Lf posterior maxilla and posterior mandibular region.
CONTRAST ENHANCED CT NECK
Expansile unilocular lytic lesion involving the maxillary arch on the left side bulging in the lumen of the left maxillary sinus
- Rx: Tab. Augmentin 625mg BD
- Rx: Inj. Cefotaxime 1gm IV/BD
- Rx: Inj. Cefotaxime 1gm IV/BD
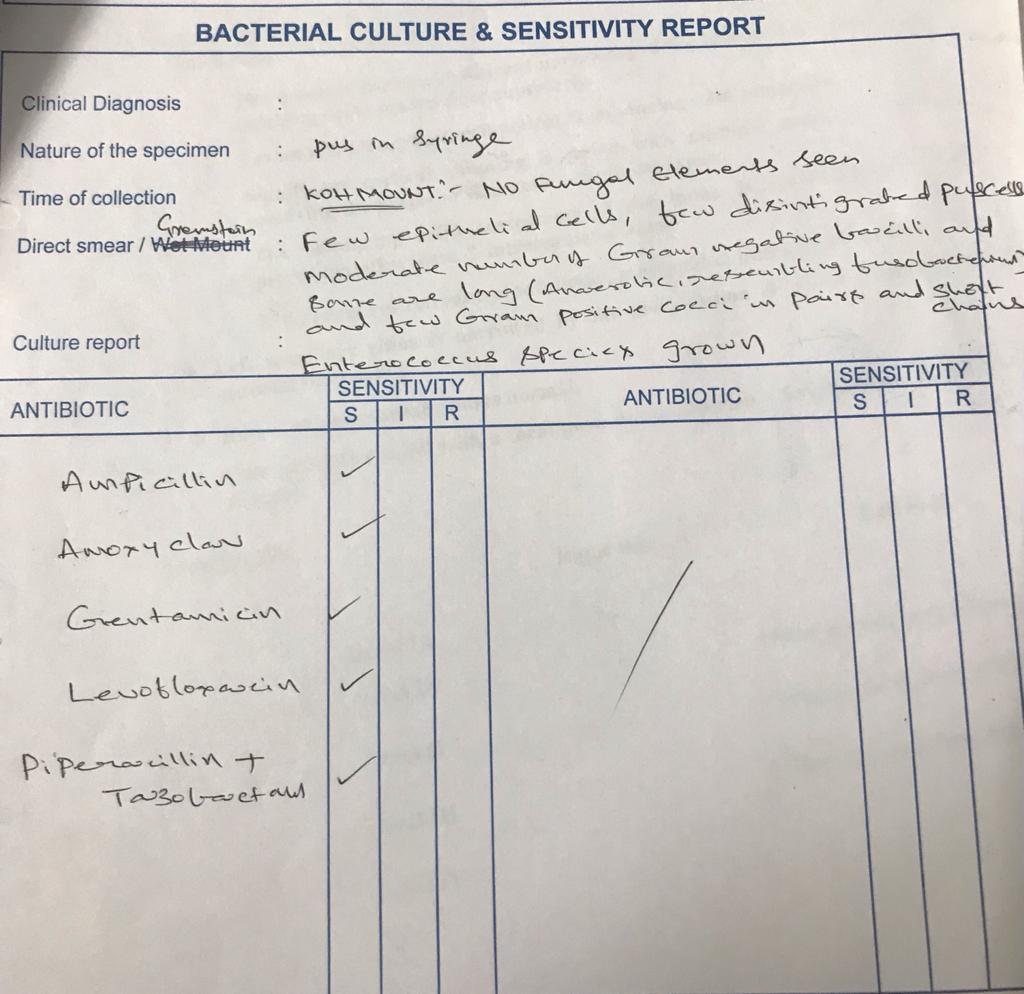
- Pus sent for culture + sensitivity test
- GRBS 102mg/dl
- Rx: Inj. Metrogyl 100ml
- GRBS 102mg/dl
- Rx: Inj. Metrogyl 100ml
- Rx: Inj. Augmentin 1.2gm IV/BD for 5 days
- Rx: Inj. Augmentin 1.2gm IV/BD for 5 days
























Comments
Post a Comment