A 22 year old woman with facial puffiness and pedal edema
This E blog also reflects my patient online learning portfolio and your valuable inputs on the comment box is welcome.
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient.
CHIEF COMPLAINTS:
A 22 year old woman who is a farmer by occupation , resident of Nalgonda came to the medicine OPD with the chief complaints of :
Facial puffiness since 5 months
Bilateral pedal edema since 5 months
Fatigue since 5 months
HOPI :
Patient was apparently asymptomatic 5 months back then she developed facial puffiness which is insidious in onset and gradually progressive in nature which is relieved on medication.
Then she has a complaint of bilateral pitting edema Since 5 months which is insidious in onset and gradually progressive in nature which is relieved on medications .
History of recurrent fever episodes and fatigue since 5 months which is relieved on medications.
COURSE OF ILLNESS :
In July 2022
Patient developed facial puffiness and bilateral pedal edema associated with fever and chills for which she visited a local hospital and prescribed with medications but the symptoms are not relieved.Then after 3-4 days she visited to our medicine OPD and underwent investigations and treated appropriately and got relieved with the symptoms.
In October 2022 :
She had typhoid fever and took medications then again she started developing pedal edema and facial puffiness .
In November :
On November 22nd she came to our OPD and prescribed with medicines but there is no improvement in the symptoms .
So again she visited our op on 29th of November and got admitted .
DAILY ROUTINE :
She wakes up around 5:30-6 am in the morning and finishes her household works by 8 am and she will have her first course of meal by 9 am and then leaves for farm work and works till 1 pm and then she will have her second course of meal and takes rest for sometime and finishes her work in the farm and goes back to home by 5:30 - 6pm and by 9 pm she will her third course of meal and goes to bed by 10 pm .
PAST HISTORY :
Not a known case of hypertension , diabetes, tuberculosis , asthma and epilepsy
No history of any surgical interventions
TREATMENT HISTORY :
Torasemide p/o BD
Paracetamol during fever episodes
No significant family history present
PERSONAL HISTORY:
Diet - mixed
Appetite- decreased
Bowel - regular
Bladder - decreased urine output
Sleep - adequate
Addictions : no addictions
And no food allergies
GENERAL EXAMINATION :
Patient is conscious , coherent and cooperative, well oriented to time place and person
Moderately built and nourished
Pallor - absent
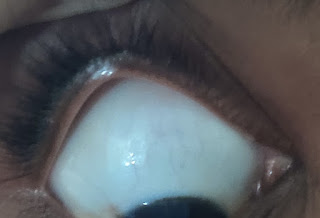
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - no palpable lymph nodes
Edema - bilateral pitting edema is present
VITALS :
Temperature - a febrile
BP - 130/80 mmhg
RR - 18 cpm
PR - 78 bpm
Spo2 - 98%
SYSTEMIC EXAMINATION :
CVS examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs.
Respiratory system :
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
Per Abdominal examination:
On Inspection
Umbilicus inverted , No abdominal distention,no visible pulsations,scars and swelling.
On Palpation
Soft, non tender, no organo megaly.
On Auscultation
Bowel sounds heard
CNS :
No focal neurological disorder found
Normal speech
TREATMENT :
1.Salt restriction (<2.4 gm/day)
2.Fluid restriction (<1 lit/day)
3.Tab.Lasix 20 mg PO /BD
4.Tab .Ramipril 2.5 mg PO/OD
No neurological deficit found.
Normal speech.














Comments
Post a Comment