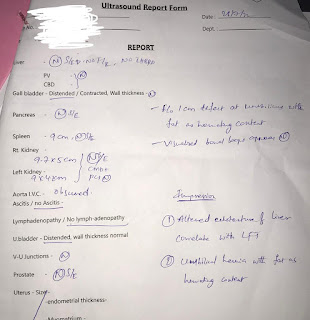
45 year old male with ascites
THIS IS AN ONLINE E LOGBOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT
45 year old male who is a resident of Nalgonda and Sheperd by occupation presented to the hospital with chief complaints of shortness of breath and cough since 6 years abdominal distention , facial puffiness , pedal edema since 3 years
HOPI
patient was apparently asymptomatic 6 year back and then he developed shortness of breath which is insidious in onset gradually progressive which is grade 2 (MMRC grading ) .
Then he developed cough which is productive with sputum which is yellow in colour and non blood stained
There is history of abdominal distention since 3 years which is insidious in onset and gradually progressive then he consulted a local doctor and used medications but then its not relieved and continued to progress for which he came here .
He also has history of facial puffiness and pedal edema for which he is on medications .
History of constipation since 1 year .
No history of vomiting , fever, jaundice , orthopnoea , PND, chest pain , palpitations , weight loss.
DAILY ROUTINE:
He wakes up in the morning by 6'o clock and goes to the work by 9'o clock after having breakfast and he will have his lunch by 1 in the afternoon and continues with the work then he goes back to home by 6 pm in the evening .
PAST HISTORY:
No similar complaints in the past
Not a known case diabetes , hypertension , asthma, TB, epilepsy
He has a H/o liver infection 1year ago which had got relieved with medication.
Treatment history:
Right IOL implantation in 2021
Family history:
Not relevant
Personal history:
Diet : mixed
Appetite-normal
Sleep-inadequate
Bowel and bladder movements-constipation since 1year,urine output is normal
Addictions-He had H/o alcohol intake since his childhood 200ml/day and abstinence of alcohol from 1year
H/o smoking since childhood 18 cigars per day
GENERAL EXAMINATION:
Patient is conscious,coherent,cooperative and well oriented to time and place.
Moderately built and nourished
Bp:130/70 mm/hg
PR:88/min
RR: 17 cpm
Temperature: afebrile
HR: 74 bpm
Pallor: absent
Icterus: absent
Cyanosis: absent
Clubbing: absent
Lymphadenopathy:absent
Pedal edema: B/L pedal edema is present
Spo2: 96%
GRBS: 205 mg/dl

















Comments
Post a Comment